12-02-2025
Patient Recruitment in Clinical Trials: A Blueprint for Success

Patient recruitment in clinical trials within the planned time is a significant challenge in drug development. It could lead to missed deadlines and higher costs, and can consume much of the development timeline. To address this, careful recruitment strategies are crucial from the start and throughout the study.
In this article:
The Significance of Patient Recruitment in Clinical Trials
Recruitment of patients is vital for the success of clinical trials. It ensures that studies stay on schedule, preventing delays affecting the overall duration. Having enough diverse participants is crucial for reliable results. Timely recruitment respects participants' time and minimizes the burden on them and researchers. It also contributes to cost-effective trials and increases the chances of regulatory approval.
Patient recruitment in clinical trials involves identifying, sourcing, and educating individuals for pre-screening and initial discussions regarding potential trial participation. This process consists of all patient-related activities on an informed consent form. The patient is deemed officially "recruited" and becomes eligible for the subsequent screening phase.
Patient Demographics and Diversity - Why Does It Matter?
Ensuring diversity in clinical trials is crucial because a drug's effectiveness can vary across populations. Also, currently, there are no guidelines mandating diversity in clinical trials. This leads to a lack of representation in research.
Genetics significantly impacts diseases and health outcomes, revealing variations among ethnic and racial groups. Failure to test drugs on diverse populations can lead to the overlooking of potential differences in efficacy. For example, studies have shown that albuterol, a common asthma inhaler, is less effective for people of African descent than those of European descent.
The persistent lack of diversity in trials stems from various challenges. Limited access is a primary barrier, as awareness and trial information are essential for participation. Many trials happen in academic hospitals that require insurance coverage. People from ethnic minorities often have less access to insurance. As a result, they are less likely to hear about these trials or take part in them.
Factors Influencing Patient Participation in Clinical Trials
-
Eligibility Criteria
Eligibility criteria are crucial for accurate data, but overly strict criteria can hinder finding qualified participants. Streamlining criteria by removing non-essential details improves inclusivity without compromising results. The FDA encourages this approach to enhance diversity in clinical trials, urging a reevaluation of exclusion criteria that lack scientific support.
Adjusting exclusion criteria ensures the participant pool mirrors real-world conditions. This will increase the treatment's effectiveness for the target population if approved.
-
Site Locations
The geographical location of clinical trial sites plays a crucial role in patient participation. Accessible and convenient site locations increase the likelihood of patient enrollment. Factors such as proximity to participants' residences, transportation availability, and the ease of reaching the trial site can significantly impact recruitment and retention rates.
-
Follow-ups
The frequency and nature of follow-up visits are essential considerations for patient participation. The burden of follow-up visits can deter individuals from joining or continuing in a clinical trial. Streamlining follow-up procedures with flexible scheduling and minimal disruption to daily life promotes better adherence.
-
Communication
Clear communication is essential for increasing participation in clinical trials. Language, knowledge, understanding, and misconceptions play a crucial role. Insufficient information, a lack of understanding, and doubts about clinical trial effectiveness discourage participation. On the other hand, providing clear and accessible information in the relevant language positively influences participants.
-
Informed Consent Process
Healthcare Professionals often view the informed consent process as a barrier to recruiting for clinical trials. Some argue that patients may find full information disclosure psychologically harmful. Meanwhile, others suggest that it could impact the trust in the doctor-patient relationship.
Clinicians might be hesitant to disclose information due to the explicit acknowledgment of uncertainty in clinical trials. However, studies show that patients often desire more information than clinicians anticipate, especially regarding their diagnosis, prognosis, and treatment options. The impact of increased information on patients remains inconclusive, with some studies suggesting it may raise anxiety levels. In contrast, others find it allows for a fully informed choice before treatment decisions.
Leveraging Technology for Clinical Trial Recruitment
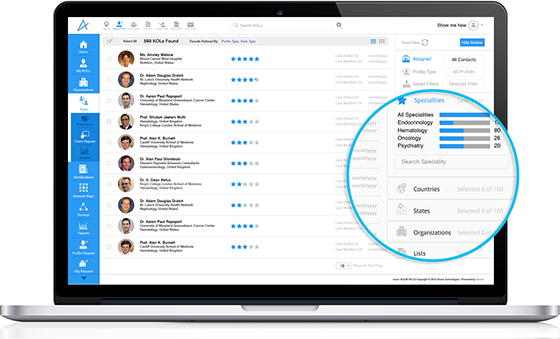
The conventional methods of identifying eligible Patients through hospitals or clinics can be inefficient when dealing with large populations. AI technology emerges as a valuable tool in optimizing the recruitment process and minimizing the need for unnecessary screening.
When provided with specific eligibility criteria, an AI-based system can analyze hospital databases and generate a targeted list of potential participants. This list is a resource for clinicians to inform eligible patients about the trial, or the automated system can directly contact patients. However, careful supervision by clinicians to prevent any undue pressure on individuals to participate is also essential.
As noted by experts, a critical aspect of leveraging AI in patient recruitment for clinical trials involves data mining techniques. Natural Language Processing (NLP) is a key player in this domain. Since the terminology in trial descriptions may be too complex for patients to grasp, NLP is crucial in translating this information into layman's terms. This translation aids in identifying eligible, well-informed, and motivated patients for potential participation in clinical trials.
Moreover, escalating expenses associated with patient enrollment have prompted sponsors, Contract Research Organizations (CROs), and patient recruitment firms to explore innovative strategies for enhancing recruitment outcomes. To address this, many organizations are turning to social media as a pivotal tool for augmenting patient enrollment.
Traditionally, drug companies (sponsors) heavily relied on print, radio, and occasionally television advertisements for clinical trial recruitment. In recent years, there has been a shift towards incorporating online clinical trial registries, company-sponsored clinical trial websites, and online patient recruitment firms into the recruitment process to bolster enrollment.
FAQs
-
How can Patient Recruitment in Clinical Trials be Improved?
Employing targeted marketing strategies, leveraging social media, collaborating with Healthcare Professionals, and offering participant-friendly trial designs can increase awareness and interest among potential participants.
-
Why Is It Difficult to Recruit Patients for Clinical Trials?
Recruiting patients for clinical trials is challenging due to limited awareness, stringent eligibility criteria, and participant reluctance. Overcoming these challenges requires targeted outreach, streamlined criteria, and transparent communication to foster trust and encourage participation.
-
What is the recruitment process in clinical trials?
The clinical trial recruitment process includes identifying eligible participants through advertising, referrals from healthcare providers, and community engagement. Interested individuals undergo screening to ensure they meet the study's eligibility criteria, and upon confirmation, informed consent is obtained before enrollment in the trial.