13 Dec 2023
Patient-Centered Care: A Pathway to Enhanced Health Outcomes

Healthcare delivery has come a long way from traditional practices of what doctors say is right to a healthcare mode that is more patient-focused. Modern research underscores the significance of adopting a Patient-Centered Care (PCC) approach in healthcare. Governments and health policy groups worldwide actively promote healthcare institutions to prioritize individual needs. The primary goal of PCC is to establish a collaborative partnership between patients, families, and healthcare providers to enhance the overall quality, effectiveness, and healthcare experience.
In this article:
Four Principles of Patient-Centered Care
Patient-centeredness in healthcare has long been acknowledged as a valuable attribute. Advocates define it as one that respects patients' preferences, needs, and values, adopting a comprehensive biopsychosocial perspective rather than a purely biomedical one. It involves establishing a robust partnership between the patient and clinician. Described below are 4 Principles of patient-centered care:
-
Respecting and Upholding Dignity
Healthcare professionals need to demonstrate respect for patients and their families by attentively listening to their perspectives and honoring their choices. The planning and delivery of care take into account the knowledge, values, beliefs, and cultural backgrounds that patients and their families bring to the healthcare setting.
-
Transparent Information Sharing
Healthcare practitioners should be committed to transparent communication and sharing comprehensive, unbiased information with patients and families. This information is conveyed in affirming and beneficial ways, ensuring that patients and their families receive timely, accurate, and complete information. This facilitates their active participation in care and decision-making processes.
-
Empowering Participation
Patients and their families should be encouraged and supported to actively participate in their care and decision-making processes at a level that aligns with their preferences and comfort.
-
Promoting Collaboration
Collaboration must extend beyond patient-practitioner interactions; it involves active engagement between patients, families, healthcare practitioners, and leaders. This collaborative effort must include policy and program development, implementation, and evaluation. It should also extend to facility design, professional education, research endeavors, and the actual delivery of care, fostering a holistic and inclusive healthcare environment.
Dimensions of Patient-Centered Care Model
A study paper published in NCBI has elucidated three dimensions of patient-centered care, which integrates a broad range of sub-topics.
-
Communication
The healthcare approach begins with attentive listening. It helps to develop a foundation of trust through clear and empathic communication customized to individual needs while encouraging the involvement of family, friends, and caregivers.
-
Knowing the Patient
Effective interactions are fostered by utilizing a comprehensive understanding of the Patient as a unique individual, establishing common ground based on their preferences, and facilitating the development of healing relationships.
-
Importance of Teams
The entire care team is responsive to patient and family needs, recognizing that the actions of both clinicians and staff significantly influence perceptions of care.
-
Clinical Decision Support
This type of care ensures shared decision-making, integrating the best-available evidence with patient preferences and offering self-management support.
-
Clinical Coordination and Continuity
Seamless care transitions and information flow are managed, with coordination extending to community resources to ensure comprehensive and continuous healthcare.
-
Types of Encounters
The healthcare system accommodates various encounters, including virtual visits (phone, email), supported by a reimbursement structure designed to meet diverse patient needs.
-
Built Environment
The physical space is designed to be calm and welcoming, accommodating the diverse needs of patients, clinicians, and families while emphasizing easy navigation within the system.
-
Access to Care
Streamlining the appointment-making process, adapting payment systems to individual circumstances, and prioritizing coordinated, consistent, and efficient care contribute to minimizing wait times.
-
Information Technology
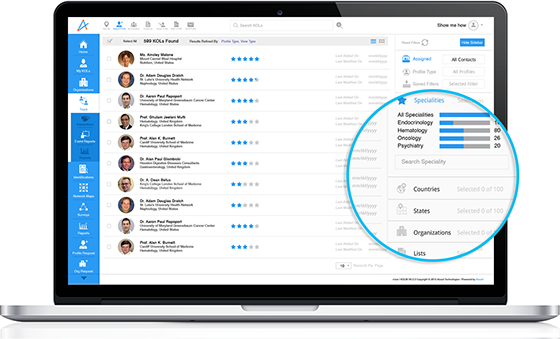
Information technology supports patients and clinicians throughout, dynamically tracking preferences, values, and needs and providing self-management tools and information for an enhanced healthcare experience.
Interpersonal Dimension
Clinical Dimension
Structural Dimension
Assessing the Impact of Patient-Centered Care within Healthcare Organizations
Assessing the impact of patient-centered care within HCOs requires a comprehensive evaluation across multiple dimensions. A study on 479 cancer patients in Singapore revealed that clear communication between patients and healthcare providers indicates a better quality of life in patients.
Also, it indicated that when patients have more chances to discuss worries or concerns, their psychosocial scores tend to be higher. The emotional support provided by healthcare providers contributes to improved emotional well-being for patients.
Moreover, when it comes to continuity of care after the transition to home, most adolescent diabetic patients reported that they did not always receive information on health symptoms to watch out for. So, this finding also suggests a service improvement that can potentially improve patient clinical outcomes. This could lead to over or under-usage of treatment modalities in people with chronic conditions such as diabetes complications.
Digital Horizons in Patient-Centered Healthcare
Digital Health includes technology-driven services aimed at enhancing patient health and well-being. It comprises various components such as:
-
Telemedicine and Telehealth are used to facilitate patient and healthcare provider engagement through telephone and video channels.
-
Digital Tools are involved in the monitoring, aggregating, and sharing of patient data with healthcare providers.
-
Mobile Health (mHealth) allows patients access to healthcare information and expertise through smartphone and tablet applications.
-
Health Information Technology empowers Healthcare Professionals to utilize algorithms and electronic health records (EHRs) for identifying, ordering, and delivering healthcare services.
-
Digital health holds the potential to access health information and enhance and offer patient-centered healthcare. It enables personalized healthcare, reduces costs, and provides patients with the opportunity for omnichannel experiences that cater to their medical and social needs.
While Technological Advancements in the Digital sphere have been known to enhance patient-centered care, their widespread adoption faces challenges. Internet access, a crucial social determinant of health, must be addressed to ensure equitable care models. Additionally, digital care models should support healthcare providers without causing burnout. Seamless transitions between different levels of digital care require learning from experiences and adapting to evolving healthcare needs.
FAQs
-
What is patient-centered care?
Patient-centered care is a healthcare approach that prioritizes the specific needs, preferences, and experiences of patients in the healthcare process. It involves fostering a partnership between healthcare providers and patients, considering their values, and involving them in decision-making to ensure a more personalized and practical care experience.
-
What are the 4 C's of patient-centered care?
The 4 Cs of patient-centered care are compassion, communication, coordination, and collaboration. These principles emphasize the importance of empathy and understanding, effective communication between healthcare providers and patients, seamless coordination of care, and collaborative efforts among the healthcare team to ensure a wholesome and patient-focused approach.
-
What is patient-centered care, and its importance?
Patient-centered care implies a healthcare approach that prioritizes patients' individual needs and preferences, involving them in decision-making and ensuring a more personalized and empathetic care experience. It is important because it helps to improve patient satisfaction and outcomes, enhance communication between healthcare providers and patients, foster trust and mutual respect, promote better adherence to treatment plans, and increase overall Quality and effectiveness of healthcare delivery.
-
What are some examples of patient-centered care that can be implemented today?
Personalized care plans, strong patient-provider communication, and empowering tools like patient portals exemplify patient-centered care, fostering individualized treatment, trust, and active patient engagement.
Healthcare Unbound
While the patient-centered care model also focuses on the patient's relationship with healthcare providers, clinicians, or care teams, much of the patient's experience extends beyond the clinic visit. It encompasses virtual medicine, peer support groups, and various information and communication technologies. Additionally, the ability of HCPs to deliver care is influenced by the specific context in which they operate, whether it be a large hospital, small private practice, freestanding urgent care facility, or an integrated multispecialty group practice.