26 Mar 2024
Emerging Frontiers in Pharmaceutical Research

Pharmaceutical research is a multidimensional, dynamic landscape that comprises a broad spectrum of activities such as drug discovery, clinical trials, pharmacology, formulation development, regulatory affairs, and post-marketing surveillance. These activities aim to develop, test, and improve medications and their delivery to enhance the healthcare of patients across the world.
In this article:
- 1. A look at the cutting-Edge Pharmaceutical Research
- 2. The Rise of Precision Medicine
- 3. Harnessing the Power of Artificial Intelligence for Drug Development
- 4. Targeting Rare Diseases - Breakthroughs in Orphan Drug Research
- 5. Revolutionizing Cancer Treatment by Exploring Immunotherapy
- 6. Overcoming Antibiotic Resistance
- 7. Shaping the Future of Pharmaceutical Research
A look at the cutting-Edge Pharmaceutical Research
The growing emphasis on developing cutting-edge treatments for previously incurable diseases has led to the continuous evolution in pharmaceutical research. Alongside significant advancements in drug development, many breakthroughs, including gene therapies and precision medicines, have helped save lives as well as improve the quality of life of individuals.
The mRNA vaccines for COVID-19 were also one the most important breakthroughs that changed the course of healthcare. The integration of different scientific disciplines, such as the CRISPR-Cas9 technology for gene editing, has opened new avenues for treating previously incurable genetic diseases. Advancements like 3D-printed organs offer hope for resolving organ scarcity issues. Let's have a look at major advancements in pharmaceutical research:
The Rise of Precision Medicine
Precision medicine enables healthcare providers to treat patients based on their characteristics rather than relying solely on generalized evidence. The benefits of this novel therapeutic method are it helps in early disease detection and the development of personalized treatment plans.
The ability to personalize care is made possible by various data collection and analytics technologies. The integration of high-throughput genotyping with electronic health records (EHRs) provides researchers with immense opportunities to derive new phenotypes from real-world clinical and biomarker data. These phenotypes, along with EHR insights, can validate the necessity for additional treatments or enhance disease diagnoses.
One of the most extensively studied impacts of precision medicine in healthcare is genotype-guided treatment. Clinicians leverage genotype information to guide dosage decisions for medications like warfarin. Additionally, organizations like the Clinical Pharmacogenetics Implementation Consortium have published genotype-based drug guidelines to assist clinicians in optimizing drug therapies using genetic test results.
Genetic prototyping of tumors helps doctors create targeted treatment plans for patients with breast and lung cancer. Precision medicine promises more accurate diagnoses, early prediction of disease risk, and tailored treatments by prioritizing each patient's safety and efficacy. The growing effort to support precision medicine worldwide is evident from the establishment of many data repositories outside of the United States, such as the UK Biobank, BioBank Japan, and the Australian Genomics Health Alliance.
Harnessing the Power of Artificial Intelligence for Drug Development
Drug discovery and development is a lengthy, expensive, and risky process that usually takes 10 to 15 years and costs over $1 to $2 billion for each new drug approval. Advancing a drug candidate to phase 1 clinical trials is a major accomplishment; however, nine out of ten candidates fail during later phases and approval.
It is also noteworthy that the 90% failure rate only applies to drug candidates that have advanced to phase 1. If we consider the preclinical stages, then the failure rate of drug development surpasses 90%.
While there could be various reasons for the failure of drug development, one needs to know that it is inherently a trial-and-error process. However, AI (Artificial Intelligence) is proving to be a game changer and is infiltrating virtually every stage of the drug development process. Various healthtech tools are integrating AI-driven functions such as 3D protein structure prediction, protein generation, protein property predictions, and molecular docking to redefine the drug discovery process.
A recent report states that AI technologies could significantly reduce time and cost by about 25–50%. Numerous success stories have validated this point, like the discovery of an A2A receptor antagonist for solid tumors and a selective serotonin reuptake inhibitor for obsessive-compulsive disorder. Other examples include molecules like RLAY-4008 for cholangiocarcinoma, NDI-034858 for psoriasis, and EVX-01 for melanoma.
In clinical trials, digital twins are changing the game. They make patient recruitment easier by simulating patient profiles. They also help improve trial designs, making them more efficient and less costly. Digital twins can simulate patient experiences without the need for invasive procedures or harm.
Digital twins are made from data collected from various sources like sensors, wearables, health records, and genetic information. These digital avatars are infused with AI models like machine learning to enable medical teams to analyze data to predict and optimize behavior. This will help streamline clinical trial execution, cut down time and improve the outcome of the trial's quality.
Breakthroughs in Rare Diseases Treatment Research
Significant advancements have been made in the past decade in rare diseases, offering hope to patients who previously had no or limited treatment options. Cystic fibrosis (CF) treatment has received FDA's approval. It targets the malfunctioning protein caused by CFTR gene mutations and will benefit patients with different mutations.
Targeted therapies for rare blood cancers like chronic lymphocytic leukemia, chronic myeloid leukemia, follicular lymphoma, acute myeloid leukemia, and multiple myeloma have improved patient outcomes.
Gene therapy is also available for a rare childhood blindness caused by a specific genetic mutation, offering hope for restoring vision.
A new treatment for transthyretin amyloid cardiomyopathy, a leading cause of heart failure in older adults, has reduced hospitalizations and increased survival rates, especially among African Americans.
Research on existing FDA-approved medications for inflammatory conditions has led to the approval of disease-modifying treatments for all types of Juvenile Idiopathic Arthritis (JIA). These treatments help slow disease progression and prevent disability in JIA patients.
Revolutionizing Cancer Treatment by Exploring Immunotherapy
In the past few years, one focal area in pharmaceutical research has been immunotherapy, which led to advancements in the treatment of various cancers.
Immunotherapy has shown promising outcomes in treating various cancers such as lung cancer, melanoma, leukemia, and lymphoma. This treatment encompasses different methods, including checkpoint inhibitors, cancer vaccines, and CAR-T cell therapy.
Checkpoint inhibitors are medications that target specific proteins on immune or cancer cells, empowering the immune system to identify and attack cancer cells. CAR-T cell therapy involves extracting T cells from a patient's blood, modifying them in labs to target cancer cells, and reintroducing them into the patient's body. Cancer vaccines on the other hand work by stimulating the immune system to identify and attack cancer cells.
Overcoming Antibiotic resistance
A breakthrough has been made by researchers, including experts from Imperial College London, in combating antibiotic-resistant bacteria responsible for human diseases like E. coli, K. pneumoniae, and P. aeruginosa. They achieved this by inhibiting a protein crucial for the bacteria to develop resistance capabilities.
Researchers noted that their approach marks a fresh perspective on tackling resistance, a pressing health issue for the scientific community. They inhibited DsbA, using certain chemicals that prevent the production of resistance proteins. The team is now focused on creating inhibitors that can be used safely in humans to achieve the same protective effect.
Shaping the Future of Pharmaceutical Research
The research details mentioned above represent only a fraction of the vast expanse of pharmaceutical research, which includes a diverse range of treatment modalities and their corresponding research endeavors. Nevertheless, this industry is full of possibilities, especially due to emerging technologies, an ever-expanding knowledge base, and heightened awareness of diseases.
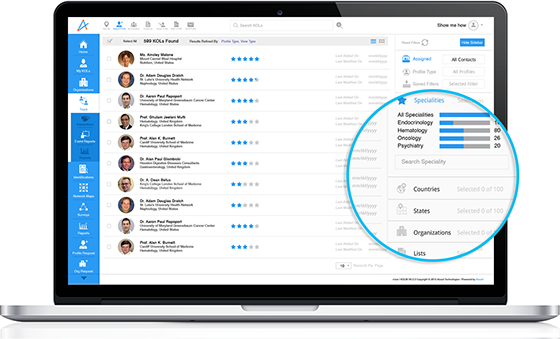
konectar, our AI-powered HCP Management Platform, empowers life sciences companies to identify investigators for clinical trials and gain valuable insights into what's happening in the clinical trial landscape. If you would like to learn more about how konectar can help propel your HCP engagement initiatives, request a demo today!